The Gardasil vaccine is achieving great success against genital warts, in what may be an early indication of similar effect against cervical cancer.
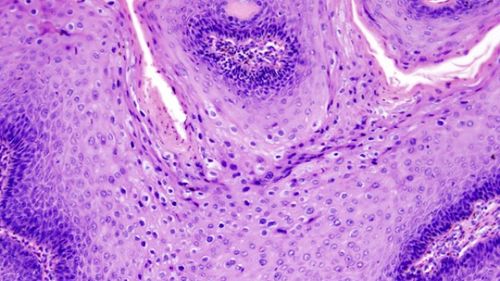
Approximately 70% cervical cancers are caused by strains 16 and 18 of the human papillomavirus (HPV). The Gardasil vaccine is designed to prevent the spread of these strains and stop cervical cancer. However, since the cancer usually takes decades to develop, it will be a long time before we can be sure the mass vaccination program has worked. Even the precancerous lesions detected in pap smears are not affected rapidly enough for those impatient to assess the vaccines' success.
What does show up much sooner after infection, however, are HPV strains 6 and 11, the most common causes of genital warts.
Consequently, Australian researchers have been studying the rate of genital warts, both to see if the vaccine proves successful against the painful and distressing condition, and as a potential proxy for future rates of cancer. So far the results have been better than anyone hoped.
The latest paper, published in PloS One indicates a 61% fall in genital warts for Australian women aged 15-27 since widespread vaccination began in 2007. The figure most likely underestimates the true impact of the vaccine since genital warts were becoming more frequent prior to Gardasil becoming available.
“The results show that the program has been a widespread success," says lead author Christopher Harrison of the University of Sydney. Harrison found that 4.33 in every 1000 visits by women ages 15 to 27 to general practitioners involved genital warts from 2004 to 2006, and this had fallen to 1.67 per 1000 from 2008 to 2012.
"For all other age-sex groups (who were not covered by the program) there was no significant change in the management rate of genital warts between the pre-program and post-program periods,” Harrison says. "There was also no significant decrease in other sexually transmitted infections over this period, which means that the decrease in genital warts was likely due to the vaccination program, not a change in the women's behavior.”
The finding follows from studies that found even more dramatic drops among women attending sexual health clinics. Those findings also demonstrated herd resistance in action, since genital warts have also fallen among hetrosexual men of the same age, even though few of them have been vaccinated.
Although Australian women have some of the highest vaccination rates in the world, almost 30% of this age group are unvaccinated. Some genital warts are caused by other HPV strains, but the findings suggest almost 100% protection against the target strains.
Gardasil is an expensive vaccine, and there has been much debate over whether providing it free is good value for public health dollars. Consequently research into Gardasil's effectiveness is important for other countries considering their options, particularly after the clinical trials were cut short even though it was showing promise.